Comforting Families Every Day
April 23, 2020 / by Jacqueline Mazarella- Alumni
As an emergency room social worker, Veronica Annette Acosta, MSW ’17, provides emotional support for families of patients who have passed away. Under normal circumstances, these conversations happen about five times a month. Under COVID-19, she is having them four times a day.
“It is extremely overwhelming,” said Acosta. “It is starting to take an emotional toll.”
Acosta has not experienced anxiety in a long time, but it has recently spouted again. She is not only providing emotional support to patients, but also the family members who are not allowed in the hospital due to current restrictions. She takes care of the patients first, and then the families who are calling, wanting to know what is happening with their loved ones.
“The anxiety is so real—there are some days you get in your car and you’re just so fearful,” Acosta said. “Outside of my line of work, outside of a nurse’s line of work, we’re also just individuals who are also dealing with this.”
Thankfully, at her hospital they now get results from COVID-19 tests in one to two hours. At the beginning of this crisis, and still in many other places, the test results were taking two weeks.
Once patients have tested positive, the doctors determine if they need to be admitted, or if they can safely go home to self-quarantine. If they are sent home, it is Acosta’s job to speak with the families and find out what accommodations can be made to keep everyone safe.
“And that is the difficult part because when you have families who maybe live in a one-bedroom, or are lower income, oftentimes there’s not a room where they are able to isolate,” said Acosta. The family members then become afraid of their own infection, and there is a huge emotional ripple effect.
Acosta’s hospital is preparing for a surge to come at the end of April, and they have already made a lot of adjustments. Now, there is a nurse at the ER entrance, instead of a security guard, who evaluates everyone upon arrival. Questions are asked related to recent travel, fever, shortness of breath and other symptoms and conditions.
They have a tent set up outside for patients suspected of being COVID-positive. Additional beds, respirators, masks, gowns and other equipment have been ordered. Medical floors are being converted into COVID only floors.
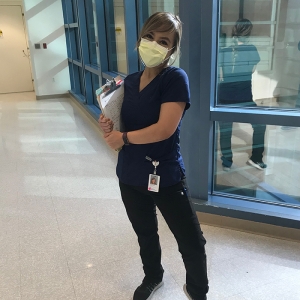
As for minimizing her own exposure, Acosta is now in scrubs and masked. “I'm wearing scrubs so I don't infect my other clothes,” Acosta said. “I change in my car and l put my clothes in a bag. I take the clothes inside and dump them into the washer. Minimize any touching! These are things I’ve learned from nurses.”
Working together
“I'm noticing that there's a lot of nurses here in the ER who are experiencing something biting, and so for me what makes me feel good is just kind of extending myself,” Acosta said. She stresses to the nurses that they are in it together, and she is also there for whatever comfort they might need in the moment.
Acosta tries to ensure that there are safe spaces at work for everyone. If someone is feeling emotional, they can go for a quick walk, separate from their role for a moment. “Just be a human for a second and just maybe scream, maybe cry, maybe walk, maybe just say it out loud,” she said.
As this situation has become more stressful, Acosta’s supervisor has been providing “mental health days” for the social workers. Acosta is trying to stay as active as possible—running, journaling, listening to music, praying and talking to her family every day. “Just making sure more than ever that those around me know that we’re all here for one another is very important to me,” she said.
As a health care professional, Acosta is isolated from friends and family because of her higher risk of spreading infection.
“As much as we’re trying to be on the front lines, we’re also on the front lines of being isolated from a lot of people,” she said. “So I think we need to lean on each other more than ever right now.”
Acosta is appreciative of being able to go through all of this with the amazing people around her. That is the positive side of it.
“In a weird way I just feel very grateful from the perspective of knowing that I work with these incredible human beings,” Acosta said. “Doctors, nurses, techs, EMTs and just seeing us all do it and trying our best to have smile on our faces.”
She thinks the role of social workers is often not understood. Not only are they the emotional support system for all the loss taking place now, but they will continue to emotionally support those dealing with loss moving forward: onset of depression and anxiety, kids readjusting to school, everyone readjusting to life outside of quarantine.
“I think the roles social workers play is so vital and this is a pivotal moment for social workers to be at policy-making tables,” Acosta said. “If we ever experience a pandemic again, how can we assure the emotional aspects for employees, patients and their families, and how can we implement change to ensure we are all more prepared next time.”
For Acosta, this is a time to think about what is important, and what might be done differently as everyone is eased back into society. She hopes that people are thinking about their long-term health, appreciating human interaction, being present in the moment and valuing being outdoors.
“At the end of every day I just thank myself for getting through the day. I know it sounds silly but literally something that I perform is, ‘thank you for getting through the day and you did it.’”
To reference the work of our faculty online, we ask that you directly quote their work where possible and attribute it to "FACULTY NAME, a professor in the USC Suzanne Dworak-Peck School of Social Work” (LINK: https://dworakpeck.usc.edu)